The Child Traumatic Stress Care Process Model (CPM) was developed through a collaboration of the Department of Pediatrics at the University of Utah and the Center for Safe and Healthy Families at Intermountain Healthcare’s Primary Children’s Hospital. This work was funded through federal grant monies allocated by the National Child Traumatic Stress Initiative (NCTSI), which is part of the Substance Abuse and Mental Health Services Administration (SAMHSA).
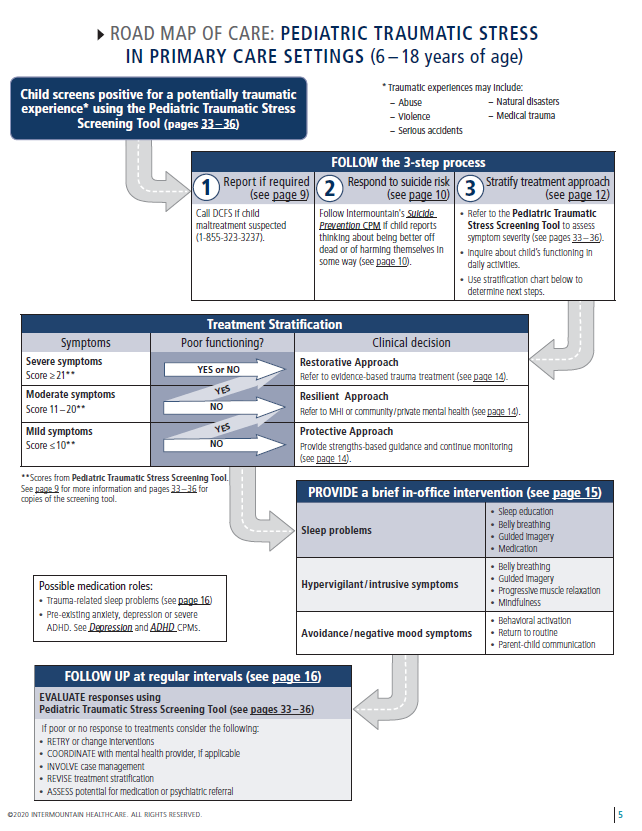
This CPM includes two processes to address child traumatic stress across the pediatric lifespan. First, primary care providers and care teams can meaningfully respond to family needs that may prevent trauma exposure in children (0‒ 5 years) through the use of the SEEK questionnaire and Road Map of Care for Pediatric Trauma Prevention. Second, primary care providers and care teams can intervene with children (6 ‒18 years) who have experienced a potentially traumatic experience through the use of the Pediatric Traumatic Stress Screening Tool and Road Map of Care for Pediatric Traumatic Stress (see image below). Continue below to learn more about the implementing the Child Traumatic Stress Care Process Model in a pediatric primary care setting.
At-a-Glance: Children 6-18 Years of Age
For children 6 – 18 years who report a potentially traumatic experience on the Pediatric Traumatic Stress Screening Tool (more information on this screening tool available in full CPM), the process of responding effectively to child traumatic stress involves three steps:
- Report if required. If the potentially traumatizing event does not involve alleged child abuse or family violence, reporting to law enforcement or child protection services is unnecessary. If abuse or family violence is the source of the potential trauma, determine if the event needs to be reported to appropriate investigative authorities. In Utah, reports can be made to either local law enforcement or the Child Protective Services (CPS) office of the Utah Division of Child and Family Services (DCFS) (1-855-323-3237). If the event has already been reported, there is no need to do it a second time.
- Respond to suicide risk. The Pediatric Traumatic Stress Screening Tool includes an item assessing recent suicidal ideation. If the parent or
youth endorses any number of days of suicidal thinking, primary care providers are directed to the Suicide Prevention CPM to determine the severity of the risk and appropriate response. Alternatively, providers can follow the included Columbia Suicide Severity Rating Scale (C-SSRS) to assess patient safety and determine response protocols, referring to local emergency medical services when needed. - Stratify treatment approach. Results from the Pediatric Traumatic Stress Screening Tool are stratified into three levels. The mild range scores (0 – 10) identify a child / teen for whom it would be appropriate to use a “protective approach” with ongoing primary care monitoring and supportive guidance building on strengths. The moderate range (11 – 20) indicates a “resilient approach” is appropriate with a brief in-office intervention and a referral to a child therapist. Scores in the severe range (21 or higher) indicate a “restorative approach” is needed, which includes a brief in-office intervention and a referral to a therapist with specialized trauma evidence-based treatments (EBT) training (in addition to safety planning, when indicated).

Brief In-Office Intervention
Based on screening tool results, a brief in-office intervention targeting their most prominent symptom(s) has been shown to make a big difference for many children. In addition to teaching them a useful coping skill, the child often feels an increased sense of support from parent(s) / guardian(s) who can help them practice the skill at home and remind them to use it when needed. For many children, belly breathing or mindfulness training (teens) will be able to slow down a racing heart or mind at bedtime to fall asleep easier or reduce the intensity of anxious / fearful or angry feelings. Children in the severe and moderate traumatic stress symptom range will typically benefit from an intervention based on their symptoms, but clinicians may also choose to use a brief
intervention with those in the low symptom range.
Follow Up at Regular Intervals
In primary care settings, you can evaluate the response to services using the Pediatric Traumatic Stress Screening Tool at follow up visits. If symptom severity remains unchanged or worsens, consider alternatives such as providing a new brief in-office intervention, reinforcing the need to follow through with treatment for those who have not, or changing the treatment stratification and therapy referral to a more intensive approach.
Why Focus on Trauma in Children
Childhood traumatic stress is the intense fear and stress response occurring when children are exposed to potentially traumatic experiences that overwhelm their ability to cope with what they have experienced. Traumatic stress needs to be addressed for the following reasons:- High prevalence. Up to 80 % of children experience at least one significant traumatic experience in childhood.
- Poor mental health outcomes. Some children and adolescents develop adverse traumatic stress responses.
- Poor health outcomes and lower life expectancy. The ACE studies link child maltreatment to early death and other poor health outcome.
- High cost. Children can experience exacerbated symptoms and poorer outcomes resulting in elevated costs.
- Often under-diagnosed and misdiagnosed.
- Early identification and integrated care using evidence-based treatments can increase positive outcomes.
Key Points
Screen for child traumatic stress. Then make 3 key decisions.
- Report if required. If abuse or family violence is the source of the potential trauma, determine if the event needs to be reported to appropriate investigative authorities.
- Respond to suicide risk.
- Stratify treatment approach.
- Mild range scores (0 – 10) “protective approach”
- Moderate range (11 – 20) “resilient approach”
- Severe range (21 or higher) “restorative approach”
Frequently Asked Questions: The Child Traumatic Stress Care Process Model
We recommend that child or caregiver complete the child traumatic stress screener while in the waiting room, prior to their appointment.
A child who is about 10 or older can complete the screener. If the child is younger than 10 or has developmental limitations, then the parent/caregiver can complete the screener for them. If the parent is completing the screener, they will receive a different version.
It’s okay to answer their questions. This is not like an IQ test or psychological testing where the results could be skewed.
The PIPS team can help you identify resources in your area. Additionally, the PIPS team has clinicians available for consultation when needed. We already have resource guides developed for many counties in Utah. Send us an email or give us a call if you have questions.
For preschool-age children, the SEEK model for pediatric primary care is recommended to guide providers in screening for, assessing, and addressing problems related to child safety. SEEK is an effective model for prevention of abuse / neglect in early childhood. It helps primary care providers identify areas of potential high risk for the child and provide relevant information and support to the parents / caregivers.
Nope. One of the best features of the child traumatic stress care process model is that it can be administered by people who don't have a clinical background. In-office interventions (such as teaching guiding imagery, belly breathing, or progressive muscle relaxation) can be taught by any individual who is comfortable teaching these skills, clinical background not necessary. Choose a skill that you are comfortable teaching and share your knowledge with the families you see in clinic.